Effects of Marijuana on Mental Health:
Depression

– Highlights
- THC and CBD appear to have antidepressant-like effects in animal models at certain doses but not others.
- Marijuana has been associated with diminished motivation, but a distinct “cannabis a motivational syndrome” has yet to be substantiated.
- Studies looking at whether marijuana use is associated with increased likelihood of development of depression have mixed findings: in some studies, associations have not been found when other variables associated with depression and marijuana use were taken into account.
- While a slight majority of medical marijuana users report using marijuana for depression and generally find it helpful, some evidence suggests that reductions in marijuana use by those with depression may actually reduce depressive symptoms.
Introduction
Marijuana is the most commonly used drug of abuse in the United States. As found in the 2015 National Survey on Drug Use and Health, 22.2 million people aged 12 and older had used marijuana in the past month. Research suggests that marijuana use has increased over the past decade as perceptions of risk of harm from using marijuana among adults in the general population have steadily declined.
As of June 2017, 26 states and the District of Columbia have enacted laws that have legalized marijuana use in some form, and additional states have recently passed measures permitting use of medical marijuana. Mental health conditions figure prominently among the
reasons given for medical marijuana use, yet there is a dearth of rigorous, experimentally controlled studies examining the effects of marijuana on mental health conditions. This research brief will summarize what is known about the effects of marijuana on depression.
Overview of Complexities in Specifying Marijuana Effects
 Any summarization of the effects of marijuana on mental health would be lacking without a brief overview of complexities in specifying marijuana effects. Unlike, say, methamphetamine, marijuana is not a single chemical compound. As a plant, marijuana is composed of more than 500
Any summarization of the effects of marijuana on mental health would be lacking without a brief overview of complexities in specifying marijuana effects. Unlike, say, methamphetamine, marijuana is not a single chemical compound. As a plant, marijuana is composed of more than 500
chemical substances. Only a fraction of these have been studied. It is generally understood that the psychotropic substance in marijuana that is primarily responsible for its intoxicating effects is
delta-9-tetrahydrocannabinol (THC).
More than 100 other compounds have been identified in marijuana that are chemically related to THC, called cannabinoids. Cannabinoids exert their effects through the relatively recently discovered endocannabinoid system; only since the late 1980s has it been recognized that humans and other mammals have cannabinoid receptors throughout the body and endogenous cannabinoids that modulate the effects of neurotransmitters and other cellular mechanisms in ways that are not yet fully understood but that have generated intense interest as potential targets for therapeutic drug development, including drugs for mental health.
Of the two known cannabinoid receptors, CB1 and CB2, CB1 is expressed abundantly in the brain and central nervous system (CNS) while CB2 expression is low in the CNS but high in peripheral immune cells and tissues.10 Psychoactive effects of marijuana are attributed to CB1 receptors whereas CB2 receptors are non-psychoactive. Aside from THC, the most studied phytocannabinoid is cannabidiol (CBD). CBD has been described as non-psychotropic due to the fact that it appears to be non-intoxicating and non-reinforcing, but it does appear to be psychotropic insofar as it appears to have pharmacological benefits with regard to anxiety, schizophrenia, addiction, and depression.
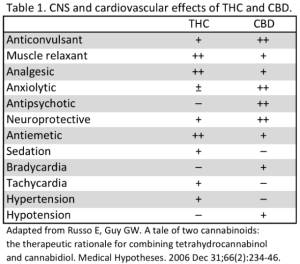
Table 1 summarizes the major CNS and cardiovascular effects of THC and CBD. CBD has been
demonstrated to attenuate certain effects of THC, including intoxication, sedation, and tachycardia. In modern clinical trials, this has permitted the administration of higher doses of THC in an effort maximize therapeutic effects while minimizing side effects. It is largely unknown how the interaction of THC and CBD plays out in practical use of marijuana by medicinal and recreational marijuana users.
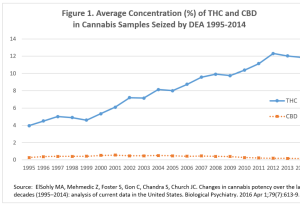
Research on cannabis products seized by the US Drug Enforcement Agency (DEA) shows that the potency of marijuana in common use has increased dramatically in the last 2 decades, at least in terms of THC content. As shown in Figure 1, from 1995 to 2014, the average THC content of seized cannabis products virtually tripled from approximately 4% to approximately 12%. On the other hand, average CBD content fell from approximately 0.28% in 2001 to < 0.15% in 2014, resulting in a change in the THC:CBD ratio of 14:1 in 1995 to approximately 80:1 in 2014.
This means that, on average, the cannabis products seized in 2014 were presumably far more intoxicating and than those seized in 1995 – and marijuana and cannabis products that are in common use may bear little resemblance to marijuana supplied by the federal government for marijuana research. In terms of strength, the
National Institute on Drug Abuse considers less than 1% to be low, 1-5% to be medium, 5-10% to be high, and over 10% to be very high.
An examination of the online menu of one of Seattle’s most popular recreational marijuana stores in June 2017 listed over 100 varieties of marijuana “flowers” that were labeled as 20% THC or higher, with THC content going as high as 30%. For many of these, CBD content was not listed. By comparison, there were only 20 varieties with listed THC content under 10%. Marijuana concentrates were labeled as having THC content as high as 97%.
From a scientific standpoint, the effects of cannabis products with such levels of THC on mental health have largely not been studied. Individual differences in objective and subjective effects of marijuana vary by individual, variety/strain, dosage, route of administration, personality, degree of tolerance, and other factors. Many of the psychological effects of cannabis and THC are biphasic and bidirectional.
Acute marijuana intoxication is generally associated with euphoria, subjective quickening of associations, relaxation, decreased motor activity, a sense of calm, increased awareness of sensory experience and internal sensations of the body, transient sensory experiences, synesthesia, craving sweet and salty foods, enhanced perception of current activities, increased salience of stimuli, simultaneous focus on multiple things, impaired shifting of focus, fantasies of power, and belief of having arrived at a transcendent insight.
With regard to neurocognition, marijuana intoxication is associated with deficits in processing speed, attention, working memory, decision-making, motivation, time-perception, and reality testing. Considering the broad range of effects, one can begin to imagine how marijuana could have beneficial or harmful effects with regard to mental health. Tolerance to certain effects of marijuana develops with regular use, within several days in some cases, as a function of CB1 receptor expression downregulation.
Research suggests that after tolerance develops it can take several weeks of THC-free recovery for CB1 receptor expression to return to baseline levels.10 Because of tolerance, the eventual downregulation of CB1 receptors with chronic use means that any benefit derived from THC with regard to mental health could result in symptom exacerbation when users are not under the influence of THC.
The Role of the Endocannabinoid System in Depression
Accumulating evidence since the 1990s indicates that the endocannabinoid system (ECS) plays an important role in regulating mood, dampening anxiety, and gating and buffering the stress response. Studies using animal models suggest that CB1 receptors are related to depression but that the role of CB1 receptors in the regulation of depressive like behavior is complex. A CB1 receptor antagonist, rimonabant, was marketed in Europe as an appetite suppressant.
It was ultimately removed from the market due to the development of depressive and anxiety symptoms in a significant proportion of patients who took the drug. Endocannabinoids appear to modulate highly interactive stress and reward networks, consisting of the ECS, dopamine system, and hypothalamo-pituitary-adrenocortical (HPA) axis. These networks establish the balance between distress and well-being. Like social interaction and exercise, marijuana intoxication produces a sought-after state of calmness or contentedness, mediated by interactive anxiolytic effects of increased cannabinoid and oxytocin receptor activation and rewarding effects of elevated dopamine.
Conversely, cannabis withdrawal is associated with lower ECS tone, partially mediated by release of stress hormones and reduced dopamine levels. Pharmacological studies in humans demonstrate that disruption of endocannabinoid signaling promotes anxiety, increases HPA axis activity, impairs reward processes in the brain, and enhances negative emotional memory biases, all of which are all hallmarks of depressive disorders. Medicinal Use of Marijuana for Depression. If blocking CB1 receptors produces depressive symptoms, it follows that activating CB1 receptors could alleviate them, i.e., that marijuana might have antidepressant effects.
A study by El-Alfy et al examined whether THC and other cannabinoids isolated from marijuana have antidepressant-like effects using well-accepted animal models of depression, including the forced swim test (FST) and the tail suspension test (TST). They found that THC exhibited antidepressant-like effects with a U-shaped dose-response. That is, while 1.25, 2.5, and 5 mg/kg were tested, only 2.5 mg/kg showed the antidepressant-like effect for both the FST and the TST. CBD and another cannabis-derived phytocannabinoid, cannabichromene (CBC), also exhibited antidepressant-like effects. As of June 2017, depression or dysthymia is not specifically listed as a qualifying condition for a medical marijuana (MM) card in any of the states that allow for medicinal use of marijuana.
A recent study surveyed 1429 MM users recruited through social media and MM dispensaries from December 2013 to January 2016 in Washington State about the conditions they used MM to treat, use patterns, perceptions of efficacy, and physical and mental health. More than half (50.3%) reported they used MM for depression. In general, participants indicated that they felt MM improved their symptoms of depression.
In 2016, Walsh et al reviewed the literature on the use of MM for depression. The researchers found cross-sectional studies of MM and depressed mood, 7of which reported improvements in depressive symptoms. Such improvements appear to be evident in studies of patients with a variety of comorbid medical conditions.
The researchers found one study that reported a positive association between depression severity and problematic MM use that suggested such an association might reflect increased MM use to address depression-related sleep disturbance. When considering marijuana for the treatment of depressive disorders, it should be remembered that regular marijuana use would result in tolerance to medicinal effects, thus increasing the risk of depression and fostering cannabis dependence. To date, there have been no reported randomized controlled trials to show sustained benefits of cannabis in the treatment of depressive disorders.
Relationship between Marijuana and Major Depressive Disorder and Dysthymia
A 2014 meta-analysis of 14 longitudinal studies of the association between cannabis use and depression examined the extent to which different patterns of use of cannabis are associated with the development of depression. Using data from over 76,000 individuals and including only studies that had controlled for baseline levels of depression, results indicated that cannabis use was associated with a modest increased risk for developing depressive disorders (odds ratio = 1.17, 95% CI 1.05-1.30) and that heavy cannabis use was associated with a stronger, but still moderate, increased risk for developing depression (odds ratio = 1.62, 95% CI 1.21-2.16).
Walsh et al noted that earlier reviews drew similar conclusions that marijuana use was associated with increased risk of depression, depressive symptoms, or depression severity in adults or adolescents but that a few cross-sectional studies have found that marijuana users report less negative affect as compared to non-users. A 2016 investigation using the US National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) with over 34,000 respondents examined prospective associations between marijuana use and risk of mood disorders, anxiety disorders, and substance use disorders in the general adult population.
In unadjusted analyses, in which covariates were not taken into account, cannabis use at Wave 1 was associated with a trend for increased prevalence and incidence of major depressive disorder and dysthymia at Wave 2. However, after adjusting for several covariates (family history of substance use disorder, disturbed family environment, childhood parental loss, low self-esteem, early onset anxiety, social deviance, education years, trauma past year, Axis I comorbidity, Axis II comorbidity, ever divorced, history of alcohol use disorder, history of other drug use disorder, history of nicotine dependence, age, gender, non-White), this trend was no longer evident. In the adjusted analysis, cannabis use at Wave 1 was associated only with substance use disorders at Wave 2.
A separate study of the same NESARC data that focused on mood disorders had similar findings but also examined the reverse relationship. These researchers found that a major depressive episode in the 12 months prior to Wave 1 was associated with an increased risk of initiation of cannabis use (adjusted odds ratio = 1.72, 95% CI 1.10-2.69), and this association was maintained when controlling for socio-demographics, substance use disorders and other psychiatric disorders.
The researchers suggested that marijuana by those with depression to represent self-medication to reduce affective symptoms. An interesting study by Grunberg et al. published in 2015 prospectively examined how temperament affected the relationship between baseline marijuana use and depression and anxiety one year later in a sample of college students.
They were specifically interested in the temperament dimension of harm avoidance (HA), which is characterized by heightened apprehension, shyness, pessimism, and inhibition of behaviors and particularly relevant for understanding depression and anxiety. Results indicated that, controlling for baseline levels of depression and anxiety, baseline HA was positively associated with later depression and anxiety only for those low in marijuana use. For those high in marijuana use, baseline HA was unrelated to later depression and anxiety.
In discussing their findings, the researchers point out that HA is associated with social inhibition and negative affective states such as apprehension and pessimism, and facilitating social interactions and coping with negative affect are among the top reported motivations for marijuana use, raising the possibility that people high in HA might use marijuana as a way to manage temperamental predispositions.
A 2016 secondary analysis of a brief, motivationally focused cannabis intervention for sexually active young adult women examined the relationship between reductions in marijuana use and depressive symptoms. Participants did not necessarily have a diagnosis of a cannabis use disorder or a depressive disorder. Results indicated that, among individuals endorsing mild or more severe symptoms of depression, reductions in cannabis use longitudinally predicted reductions in depressive symptoms. Reductions were considered modest but clinically meaningful.
A motivational Syndrome
Marijuana has long been associated diminished motivation, not unlike what is observed in some manifestations of depression. In 1968, a syndrome called “cannabis a motivational syndrome” was proposed by McGlothlin and West, based on conspicuous apathy and diminished ability to concentrate, follow routines, or successfully master new material observed in those who consumed marijuana frequently.
While there exists both preclinical and clinical evidence supporting the view that cannabis use is associated with an a motivational state, considerable research has failed to identify a cannabis-specific motivational syndrome and its existence remains controversial. A 2017 study by Lac and Luk sought to elucidate a motivational syndrome by examining connections between marijuana use and self-efficacy constructs of initiative, effort, and persistence.
Results showed that marijuana intake was significantly and longitudinally related to lower initiative and persistence in their college student sample.
Conclusions
In summary, the effect of marijuana on depressive disorders is complex. The endocannabinoid system appears to play an important role in regulating mood at least in part via highly interactive stress and reward networks. Marijuana has long been associated diminished motivation, but a distinct “cannabis a motivational syndrome” has yet to be substantiated. The two primary active ingredients of marijuana, THC and CBD, appear to have antidepressant-like effects in animal models at certain doses but not others.
While a slight majority of MM users report using marijuana for depression and generally find it helpful for that purpose, some evidence suggests that reductions in marijuana use
by those with depression may actually reduce depressive symptoms. Studies examining whether marijuana use is associated with increased likelihood of development of depression have produced mixed findings. In some studies, associations have not remained when other variables associated with depression and marijuana use were taken into account.
One reason for equivocal findings may be that individual differences such as temperament affect the relationship between marijuana and depression. Some marijuana users with or prone to depression do appear to derive some benefit from using marijuana. However, well-controlled studies indicate that marijuana use is associated with development of substance use disorder.

